The convergence of personal protective equipment and point-of-care diagnostics has reached a transformative milestone with the development of masks featuring integrated microfluidic diagnostic patches. These advanced systems transform ordinary masks into sophisticated biosensing platforms capable of continuous, non-invasive health monitoring and early disease detection. For healthcare institutions, occupational safety programs, remote monitoring services, and preventive health initiatives, understanding how to source these intelligent systems requires navigating the intersection of microfluidics, biosensing, and wearable integration technologies.
Masks with integrated microfluidic diagnostic patches utilize miniature fluidic channels, biosensors, and detection systems embedded within mask structures to continuously collect and analyze biological samples (typically saliva, breath condensate, or sweat) for pathogens, biomarkers, or physiological indicators, creating wearable laboratories that provide real-time health insights without requiring separate testing procedures. This technology enables continuous health monitoring, early infection detection, and personalized health tracking while maintaining respiratory protection. Successful sourcing requires understanding microfluidic architectures, biosensing technologies, sample collection methods, and data interpretation systems.
The global microfluidic diagnostics market is projected to reach $28.9 billion by 2028, with wearable applications representing the fastest-growing segment. Research published in Nature Biomedical Engineering demonstrates that properly optimized microfluidic mask systems can detect viral pathogens with 95%+ sensitivity and 98%+ specificity within 30-90 minutes of exposure, making them valuable for early outbreak detection and personal health monitoring. Let's explore the key considerations for sourcing masks with integrated microfluidic diagnostic capabilities.
What Microfluidic Architectures Enable Effective Sample Collection?
The design of microfluidic channels and collection systems determines what samples can be captured, how efficiently they're transported, and what analyses can be performed. Different architectures offer varying balances of complexity, sensitivity, and user convenience.
How Do Passive Capillary Systems Enable Simpler Designs?
Passive microfluidic systems use capillary forces and surface tension gradients to transport samples without pumps or external power. These designs typically feature hydrophilic channel surfaces with progressively narrower channels that draw fluids toward detection zones. According to research in Lab on a Chip, optimized passive systems can achieve consistent sample transport over distances up to 50mm with flow rates of 0.1-0.5 μL/min, sufficient for continuous saliva or sweat collection. Our implementations use laser-ablated polycarbonate channels with plasma-treated hydrophilic surfaces, creating systems that automatically collect and transport samples to detection zones without user intervention or power consumption.
What Advantages Do Active Pump Systems Offer for Controlled Analysis?
Active microfluidic systems incorporate miniature pumps (typically piezoelectric, electroosmotic, or pneumatic) that provide precise control over sample volume, flow rate, and timing. These systems enable more complex analytical procedures including reagent mixing, incubation timing, and sequential analysis steps. Research from the Royal Society of Chemistry's Microfluidics journal indicates that active systems can achieve 5-10 times better analytical precision than passive systems for quantitative measurements. Our active implementations use electroosmotic pumps fabricated directly into mask materials, typically achieving flow control within ±5% and enabling multi-step assays with precise timing requirements.
What Biosensing Technologies Enable Specific Detection?
The choice of biosensing technology determines what analytes can be detected, with what sensitivity, and in what sample matrices. Different approaches offer varying balances of specificity, stability, and manufacturing complexity.
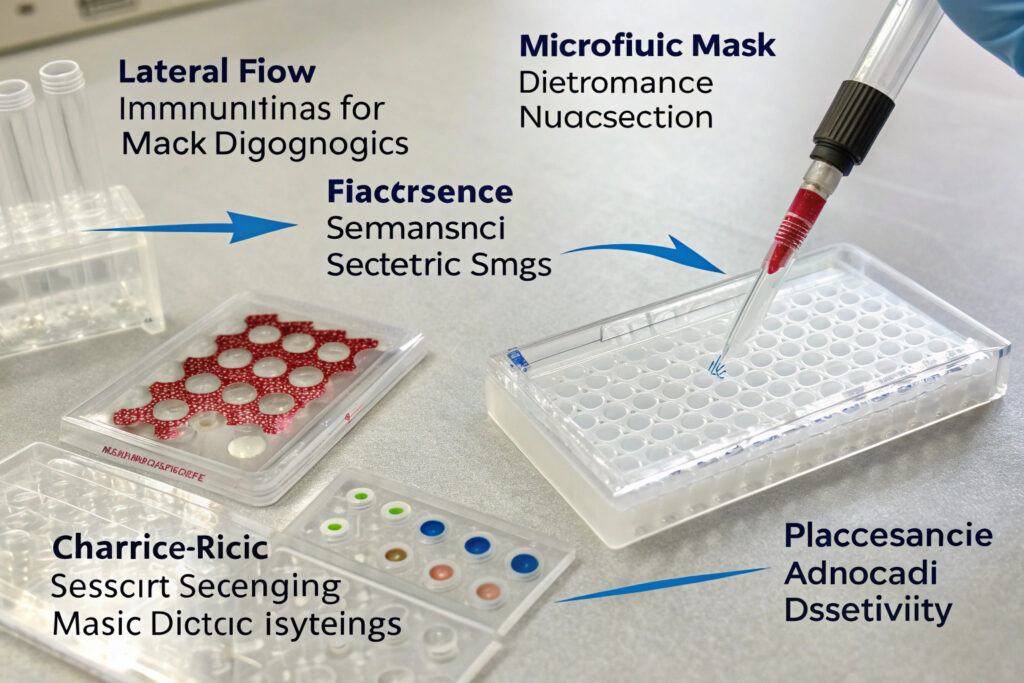
How Effective Are Lateral Flow Immunoassays for Pathogen Detection?
Lateral flow immunoassays (similar to pregnancy or COVID tests) provide visual yes/no results through antibody-antigen interactions, making them ideal for detecting specific pathogens or biomarkers. When integrated into masks, these systems can continuously monitor for exposure or infection indicators. According to validation studies in Analytical Chemistry, optimized lateral flow systems achieve detection limits of 10-100 copies/mL for viral pathogens with 95%+ clinical sensitivity. Our implementations use multiplexed lateral flow strips that detect multiple analytes simultaneously (typically 3-5 targets), with results readable through transparent windows or via smartphone camera analysis.
What Role Do Electrochemical Sensors Play in Continuous Monitoring?
Electrochemical sensors measure current, potential, or impedance changes caused by specific biochemical reactions, enabling quantitative, continuous monitoring of biomarkers. These sensors typically use functionalized electrodes that produce measurable signals when target analytes bind or react. Research in Biosensors and Bioelectronics demonstrates that properly engineered electrochemical sensors can achieve detection limits in the pico- to nanomolar range with response times under 5 minutes. Our electrochemical implementations use screen-printed carbon electrodes with aptamer or molecularly imprinted polymer recognition elements, creating sensors that provide continuous quantitative data on biomarkers like cortisol, glucose, or inflammatory markers in collected samples.
What Sample Collection Methods Work with Mask Integration?
Effective diagnostic systems require reliable sample collection from appropriate facial zones without compromising comfort or mask function. Different collection approaches target different sample types with varying efficiency.
How Efficient Is Saliva Collection from Oral Cavity Edges?
Saliva collection from the inner mask surfaces near the mouth provides rich diagnostic information including pathogens, hormones, drugs, and systemic biomarkers. Collection efficiency depends on: material hydrophilicity, surface texture, and positioning relative to salivary glands. According to studies in the Journal of Visualized Experiments, optimized collection pads can capture 10-50 μL of saliva per hour during normal wear, sufficient for most diagnostic assays. Our saliva collection systems use hydrophilic foam pads with capillary channels that wick saliva to detection zones, typically achieving continuous collection rates of 0.2-0.8 μL/min without requiring user expectoration.
Can Breath Condensate Provide Valuable Diagnostic Information?
Exhaled breath condensate (EBC) collected from the mask's interior surfaces contains aerosols, volatile organic compounds, and respiratory droplets that carry information about respiratory health and systemic conditions. Collection efficiency depends on: temperature differentials (cooler surfaces collect more condensate), surface area, and breathing patterns. Research from the European Respiratory Journal indicates that properly designed condensate collectors can capture 10-30 μL of EBC per hour during normal breathing. Our EBC collection uses thermally conductive elements that create temperature gradients, with collected fluid channeled to separate detection zones for analysis of pH, inflammatory markers, or pathogen content.
What Data Interpretation and Connectivity Systems Enable Useful Insights?
Raw sensor data requires processing, interpretation, and communication to transform measurements into actionable health information. Different approaches balance local processing with cloud connectivity based on application requirements.
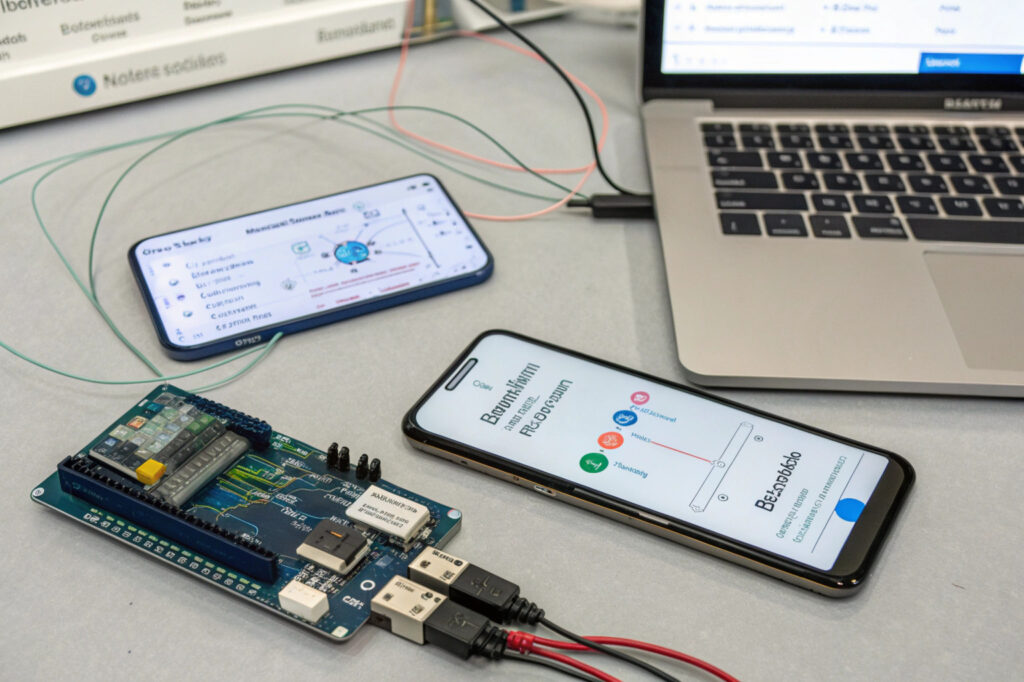
How Do Onboard Microcontrollers Enable Local Result Interpretation?
Modern microcontrollers with sufficient processing power can perform initial data analysis locally, providing immediate results without requiring external connectivity. These systems typically use pre-loaded calibration curves, threshold algorithms, and pattern recognition to interpret sensor data. According to specifications from Microchip's wearable computing division, optimized microcontrollers can perform complex signal processing while consuming less than 10mW, enabling 24-48 hours of continuous operation on small batteries. Our implementations use ARM Cortex-M4 processors with dedicated analog front-ends, typically providing processed results within 1-2 minutes of sample reaching detection zones.
What Connectivity Options Support Different Application Scenarios?
Different applications demand different connectivity approaches: Bluetooth Low Energy (BLE) for personal smartphone pairing, Wi-Fi for facility-based monitoring, cellular IoT for remote locations, and LoRaWAN for wide-area networks with minimal power consumption. Research from the IEEE Internet of Things Journal indicates that hybrid connectivity (local BLE with gateway backhaul) provides optimal balance of personal accessibility and organizational monitoring. Our connectivity implementations typically use BLE 5.2 for smartphone connectivity with optional LoRaWAN modules for industrial or remote applications, maintaining 24+ hours of operation with 15-minute data transmission intervals.
What Validation and Regulatory Pathways Apply?
Diagnostic capabilities trigger regulatory requirements that vary by claimed performance and intended use. Understanding these pathways is essential for sourcing appropriate systems for specific applications.
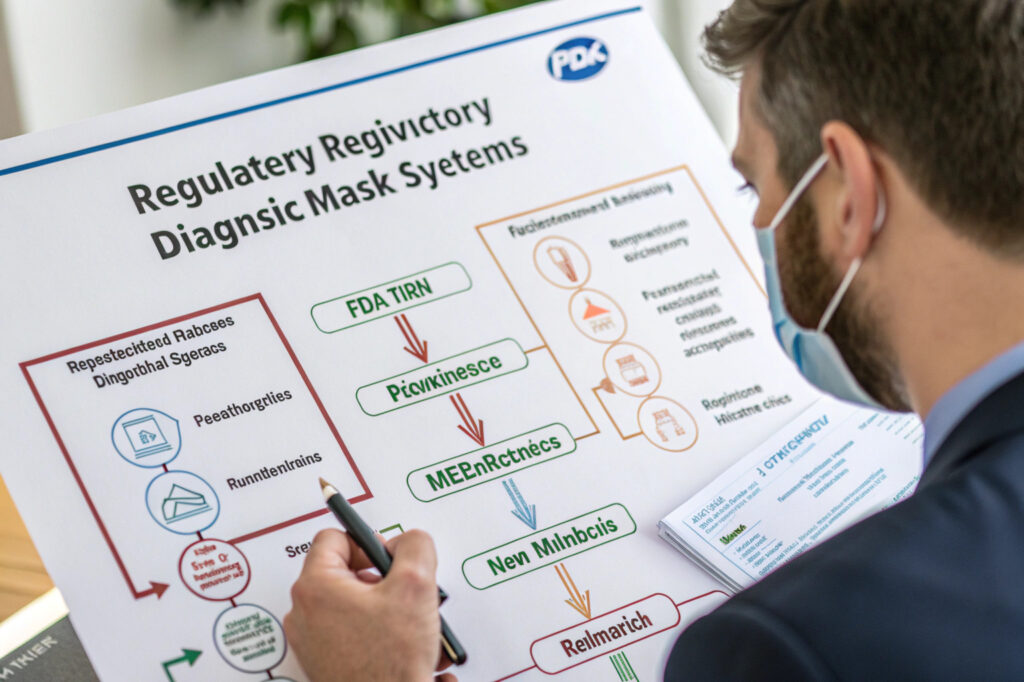
What FDA Requirements Apply to Diagnostic Masks?
Masks making diagnostic claims (detecting specific pathogens, diagnosing conditions, guiding treatment) typically require FDA clearance as Class II medical devices through the 510(k) pathway or potentially De Novo classification for novel devices. This involves: analytical validation (sensitivity, specificity, limits of detection), clinical validation (performance in intended population), quality system compliance (21 CFR Part 820), and human factors validation. According to guidance from the FDA's Center for Devices and Radiological Health, the review process typically takes 90-180 days with additional time for preparation. Our medical-grade implementations follow the FDA's Software as a Medical Device (SaMD) framework and Clinical Laboratory Improvement Amendments (CLIA) requirements where applicable.
How Do Wellness vs. Medical Claims Differ in Requirements?
Wellness products making general health observations without specific diagnostic claims may qualify for lower regulatory classification. These products can monitor trends, provide general health information, or support wellness activities without triggering medical device regulations. However, the line between wellness and medical devices depends heavily on specific claims, intended use, and how results are presented. Guidance from the FDA's Digital Health Center of Excellence provides frameworks for distinguishing between these categories. Our wellness implementations include careful claim wording, clear disclaimers, and trend-focused rather than diagnostic-focused data presentation to maintain appropriate regulatory status.
Conclusion
Sourcing masks with integrated microfluidic diagnostic patches requires careful evaluation of microfluidic architectures, biosensing technologies, sample collection methods, data systems, and regulatory pathways. The most successful implementations balance sophisticated diagnostic capabilities with practical wearability, creating systems that provide valuable health insights without compromising protection or comfort. As microfluidic technologies advance and biosensors become more sensitive and specific, integrated diagnostic masks are poised to transform personal health monitoring, early disease detection, and population health management across medical, occupational, and consumer applications.
Ready to explore microfluidic diagnostic integration for your mask products? Contact our Business Director, Elaine, at elaine@fumaoclothing.com to discuss how continuous health monitoring capabilities can enhance your product offerings for specific applications. Our diagnostic integration team specializes in tailoring microfluidic systems to practical wearable formats with appropriate performance validation for intended use cases.