The fusion of biotechnology with personal protective equipment is ushering in a new era of proactive environmental health monitoring. Masks integrated with environmental DNA (eDNA) sensors represent a groundbreaking advancement, transforming passive respiratory protection into active, mobile laboratories capable of detecting airborne pathogens, allergens, and biodiversity indicators in real-time. For procurement specialists, public health organizations, and environmental monitoring agencies, understanding how to source these sophisticated bio-sensing systems requires navigating an emerging field at the intersection of molecular biology, microfluidics, and wearable technology.
Masks with integrated environmental DNA sensors are intelligent monitoring platforms that actively sample airborne particles, extract and analyze genetic material (eDNA) from specific biological targets—such as viruses, bacteria, fungi, or pollen—and provide species-level identification through on-board or cloud-connected analysis, enabling real-time alerts and spatial mapping of biological threats. This technology shifts detection from centralized laboratories to distributed, wearable networks, offering unprecedented granularity in environmental surveillance. Successful sourcing demands evaluation of sampling efficiency, molecular assay robustness, data connectivity, and practical usability.
The global biosensor market is projected to exceed $36 billion by 2028, with environmental monitoring as a key growth driver. Research in Nature Biotechnology demonstrates that optimized eDNA capture from air can detect viral presence with sensitivity comparable to some stationary air samplers. For applications ranging from pandemic early warning to allergy management and biodiversity tracking, these masks offer a powerful, decentralized tool. Let's explore the critical considerations for sourcing this next-generation protective equipment.
What eDNA Capture and Sampling Technologies Are Most Effective?
The first challenge is efficiently capturing airborne biological particles—which carry the target DNA—onto a surface where they can be lysed and analyzed. Different sampling methods balance flow rate, particle size selectivity, and power requirements.
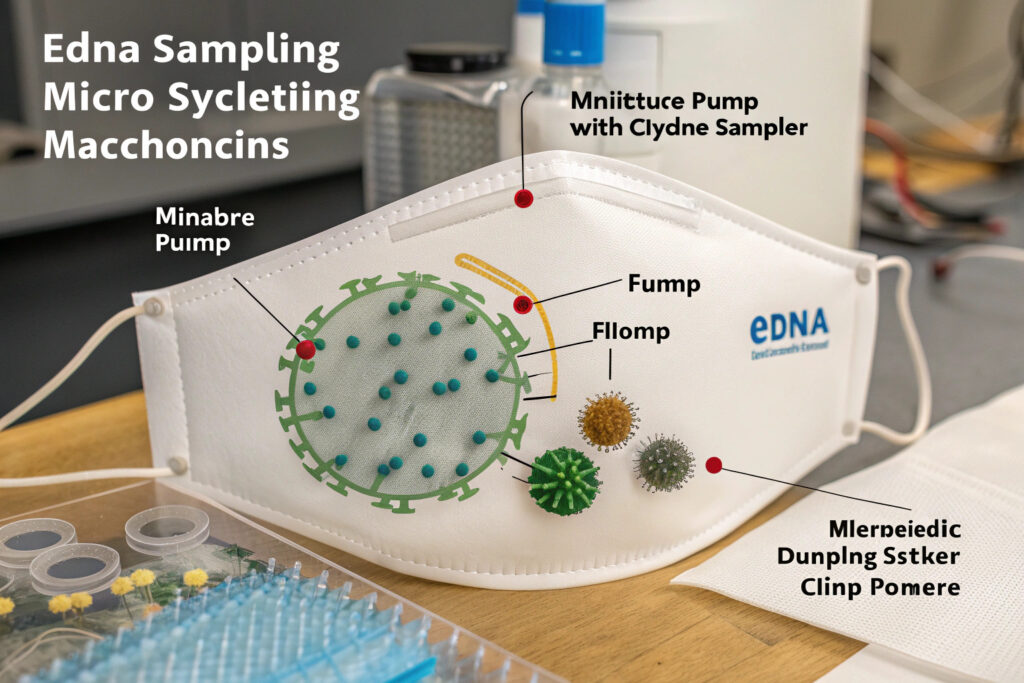
How Do Microfluidic Impactors and Cyclone Samplers Work?
These are miniaturized versions of technology used in industrial air samplers.
- Microfluidic Impactor: Air is drawn through a micro-channel and forced to make a sharp turn. Inertial forces cause particles above a certain size (e.g., >0.5 µm) to impact onto a coated collection surface within the chip. This method allows for size-selective sampling.
- Cyclone Sampler: Air is spun in a miniature vortex. Centrifugal force drives particles to the outer wall where they slide down into a collection vial or onto a surface. It is efficient for collecting a wider size range of particles with relatively low power.
According to specifications from companies like Sartorius in air monitoring, proper miniaturization can achieve sampling rates of 1-5 liters per minute—sufficient to capture meaningful eDNA over minutes to hours of wear. Our prototype integrates a low-power, piezoelectric micro-pump that draws air across a functionalized polycarbonate membrane, optimized for capturing virus-sized particles.
What is "Passive" vs. "Active" Sampling in a Mask Context?
- Active Sampling: Uses a small pump to pull a measured volume of air through the collection medium. This provides quantitative data (e.g., genome copies per liter of air) but consumes battery power.
- Passive Sampling: Relies on the wearer's inhalation to deposit particles on a strategically placed collection pad (e.g., within the exhalation valve or on the inner surface). This is simpler and requires no power but is less quantitative and more variable.
For most serious surveillance applications, active sampling is necessary to generate reliable, comparable data. Sourcing should focus on systems with efficient, quiet pumps and calibrated airflow.
What On-Device Molecular Assay Methods Are Viable?
Once particles are collected, the genetic material must be extracted, purified, and analyzed to identify target organisms. Performing these steps on a wearable device is the core technical hurdle.
Can Isothermal Amplification (like LAMP/RPA) Replace PCR on a Mask?
Traditional PCR requires precise thermal cycling (heating and cooling), which is energy-intensive and challenging to miniaturize. Isothermal amplification techniques like LAMP (Loop-Mediated Isothermal Amplification) or RPA (Recombinase Polymerase Amplification) are game-changers for wearables. They amplify target DNA sequences at a single, constant temperature (e.g., 60-65°C).
- Advantages: Much simpler instrumentation (only a heater is needed), faster (results in 10-30 minutes), and more tolerant of sample impurities.
- Integration: These reactions can be performed in pre-loaded, disposable microfluidic cartridges with lyophilized (freeze-dried) reagents. The mask's electronics need only to heat the chamber and read the result.
Suppliers developing such cartridges for point-of-care diagnostics, like TwistDx (for RPA), are key technology enablers. Our development uses a LAMP-based assay cartridge that snaps into the mask, providing results for up to 10 common respiratory pathogens in under 20 minutes.
What Detection Methods Provide Readable Results?
After amplification, the presence of target DNA must be detected. Options suitable for wearables include:
- Colorimetric Change: A pH indicator or dye that changes color visibly (e.g., from pink to yellow). This allows for simple visual readout by the user.
- Fluorescence: A more sensitive method where a fluorescent dye is excited by an LED and detected by a photodiode. This requires integrated optics but enables quantitative measurement and multiplexing (detecting multiple targets).
- Electrochemical: DNA probes on an electrode change the electrical current when the target binds. This is highly integrable with electronics.
For a mask, a dual approach is often best: a simple colorimetric result for the user and a more precise fluorescent or electrochemical readout that is logged digitally and can be transmitted.
What Data Management and Connectivity Infrastructure is Needed?
A single eDNA sensor mask provides personal awareness; a network of them provides powerful epidemiological or environmental mapping. Thus, data handling and connectivity are critical components.

How is Privacy Protected in a Distributed Biosurveillance Network?
Collecting location-tagged health data is highly sensitive. A robust system must implement:
- On-Device Anonymization: The mask or phone app should replace personal identifiers with a random, rotating ID before transmission.
- User Consent & Control: Clear opt-in procedures and user dashboards to control what data is shared.
- Data Minimization: Transmitting only essential data (e.g., "Influenza A detected at [grid location]" rather than "John Smith has the flu").
- GDPR/CCPA Compliance: Adherence to regional data protection regulations.
Sourcing should include a review of the supplier's data governance policies and technical architecture for privacy-by-design.
What Role Does Geotagging and Spatiotemporal Analysis Play?
The power of mobile eDNA sensing is mapping the presence and spread of biological agents. Therefore, each sensor reading must be tagged with:
- Time: Precise timestamp.
- Location: GPS coordinates (from the paired smartphone).
- Environmental Context: Optional data from other onboard sensors (e.g., temperature, humidity, PM2.5) that can influence results.
This data, when aggregated, allows health authorities to identify hotspots, track dispersion, and model transmission dynamics in ways static sensors cannot. The cloud platform must be capable of real-time spatiotemporal analysis.
What Are the Key Performance and Validation Metrics?
Unlike standard masks, eDNA sensor masks are diagnostic devices. Their performance must be validated with the same rigor applied to laboratory tests.

How are Sensitivity and Specificity Measured for Airborne eDNA?
- Sensitivity (Limit of Detection - LoD): The lowest concentration of target organisms in air (e.g., virus copies per cubic meter) that the mask can reliably detect. This is determined by testing in controlled aerosol chambers with quantified challenges.
- Specificity: The ability to correctly identify the target and not give positive results for non-target organisms. This is tested by challenging the mask with a panel of related and unrelated biological aerosols.
Suppliers should provide validation data from independent laboratories following guidelines akin to the CDC's Laboratory Testing Guidelines or CLSI standards. Ask for the Clinical Evaluation Report.
What is the Sample-to-Answer Time and Duty Cycle?
- Sample-to-Answer Time: The total time from starting the air sampler to receiving a result. For actionable surveillance, this should ideally be under 30-60 minutes.
- Duty Cycle: How often can a test be run? This depends on cartridge capacity (single-use vs. multi-use) and battery life. A mask intended for all-day monitoring might sample and analyze air every 2-4 hours.
Understanding these operational parameters is essential for planning deployment in field studies or occupational settings.
Conclusion
Sourcing masks with integrated environmental DNA sensors requires evaluating a complete system: efficient and quantitative air sampling, robust on-chip molecular biology using isothermal amplification, clear detection methods, and secure data infrastructure for geospatial mapping. The most viable systems will balance high performance with practical wearability, using disposable assay cartridges and efficient power management. As this technology matures, it promises to democratize environmental biosurveillance, creating a real-time, human-powered network for detecting everything from pandemic viruses to invasive species and allergenic pollen.
Ready to explore the frontier of biosensing personal protective equipment? Contact our Business Director, Elaine, at elaine@fumaoclothing.com to discuss pilot programs, sourcing, or co-development of masks with integrated eDNA sensors for your specific monitoring applications.